Sexual Dysfunction and the Male Pelvic Floor
Summary
The muscles of the pelvic floor are essential to healthy sexual function. "In women and men, the pelvic floor is an active sexual organ."[1] Its role in sexual dysfunction, however, is often underestimated or overlooked. Maintaining good muscle tone and the ability to fully contract and relax these muscles improves sexual functioning and and enhances the perception of pleasure. Conversely, chronic tension or persistent weakness can lead to dysfunction and pain, as well as a diminished sensory experience and lack of sexual feelings.
"Recently, musculoskeletal factors have been recognized as significant contributors to the mechanism of pelvic pain and associated sexual dysfunction, and in particular, pelvic floor muscle hypertonus [tension] has been implicated" according to an article in the Journal of Sexual Medicine[2]. In her 2009 book Heal Pelvic Pain, Amy Stein states that "studies have shown that more than 90 percent of men who suffer pelvic pain also experience sexual dysfunction, and that more than half of them improved their sexual function through massage of the pelvic floor muscles and relaxation techniques."[3] Rosenbaum and Owens agree, reporting that "manual techniques, including massage, stretching, and soft tissue and bony mobilizations are important components of treatment..."[2]
Below are several categories of male sexual dysfunction, including Erectile Dysfunction ♦ Painful Ejaculation ♦ Premature Ejaculation ♦ Pain in the Penis ♦ Chronic Scrotal / Testicular Pain ♦ Anodyspareunia/Male Dyspareunia: Painful or Difficult Receptive Anal Sex ♦ and Pelvic Pain as Sexual Pain. The relevance of the pelvic floor muscles is discussed in each section, as well as the role that massage and bodywork, pelvic floor muscle exercises, or both can play in improving these conditions. At the end of each section on the right side are "back to top" links to return to the main menu.
Hover your cursor over citation numbers to view the source in a pop-up text box or scroll to the bottom of the page for the full list.
→ Note that I work with a number of additional genital and sexual conditions, dysfunctions, and syndromes not specifically discussed in the text below, including but not limited to:
- Hard Flaccid
- Penile retraction and/or constriction: inward pull or compression at the base of the penis often resulting in discomfort or pain and reduced penile length
- Cremaster muscle tension, spasm, or hyperactivty: excessive or uncomfortable upward contraction of the testicles toward the groin and abdomen (Cremasteric Synkinesia and adult Retractile Testis are among the potential medical diagnoses)
- Tight foreskin: excess tension, restriction, and a lack of mobility of the foreskin (often referred to as adult, or pathologic, phimosis)
- Pain, discomfort, or dysfunction related to use, misuse, or overuse of sex toys and devices
- Pelvic floor, genital, and sexual pain, dysfunction, or altered sensation related to physical, emotional, or sexual abuse
- Restless Genital Syndrome / Persistent Genital Arousal Disorder: intrusive or unwanted genital sensations or restlessness, usually associated with arousal but in the absence of sexual desire or activity
- Soft Glans Syndrome, also known as Floppy Glans Syndrome or Cold Glans Syndrome
- Urinary and sexual dysfunction related to prostate procedures or surgery
- Genital or sexual pain, discomfort, or dysfunction related to other pelvic or abdominal medical procedures or surgeries
Erectile Dysfunction (ED)
"Approximately 80% of cases of erectile dysfunction are due solely or predominantly to organic [physical] causes" state Siroky and Azadzoi in the book Pelvic Floor Disorders.[4] The physical process of erection is largely a vascular event, initiated and assisted by the nervous system. Simply put, adequate blood must flow into the penis, and it must be trapped there to create and maintain rigidity. This process is facilitated by the pelvic floor, especially the bulbospongiosus (sometimes called bulbocavernosus) and ischiocavernosus muscles, which are instrumental in exerting tension on the penile connective tissues to block, or occlude, the emissary and deep dorsal veins that drain the penile tissues. When weak, these muscles cannot effectively inhibit this outflow, resulting in partial or total flaccidity, or ED. "It has been shown that contractions of the ischiocavernosus (IC) and bulbocavernosus (BC) muscles are very important in the process of penile rigidity" say Sommer et al.[5] In another study, Colpi and colleagues report that "our results clearly demonstrated that a reduction of contractile activity of the perineal muscles [IC and BC] may be related to erectile dysfunction."[6] Bo et al. agree: "Weak pelvic floor muscles compromise penile erection"[7], as do Carriere and Feldt: "An increasing ability to contract and relax the pelvic floor improves sexual functioning in men with erectile dysfunction."[1]. Ballard reviews a number of studies that report similar findings[8].
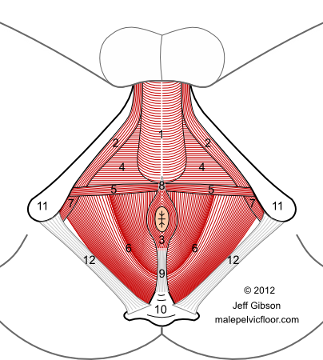
The pelvic floor muscles viewed from below. Note the Bulbospongiosus (1) and Ischiocavernosus (2). See my Anatomy page for a larger size and full labeling.
Exercises for the pelvic floor with a focus on these two muscles have proven to be very beneficial for ED. "Pelvic floor exercises are very effective in treating erectile dysfunction." state Dorey et al.[9] They conclude with "... pelvic floor muscle exercises should be considered as a first-line approach for men seeking long-term resolution of erectile dysfunction without acute pharmacological and surgical interventions that might have more significant side effects. Men demanding a 'quick fix' or a 'pill for every ill' might prefer to restore normal muscle function once they understand the important role of the pelvic floor muscles." Sommer's study[5] found that 80% of men in the pelvic floor exercise group reported "better erections", whereas 74% of the PDE5-inhibitor group (Viagra, e.g.) reported better erections. The exercise program he used in the study was based on his VigorRobic protocol, outlined in his book VigorRobic: Increased Potency Through Specific Fitness Training.[16] When considering pelvic floor exercises vs other treatments, Van Kampen et al. propose this sensible approach: "Starting therapy with the least invasive option seems a logical strategy. Pelvic floor exercises do not involve any risks, and they are painless."[10]
My pelvic floor work will help you become aware of these muscles, including the bulbospongiosus and ischiocavernosus. You will learn how to contract the entire pelvic floor with an emphasis on these two muscles, and I will give you a home exercise protocol for improving strength and tone. Beyond its specific influence on ED, a strong yet supple pelvic floor can enhance overall sexual response and the experience of pleasure.
For those men whose ED is associated with Chronic Prostatitis / Chronic Pelvic Pain Syndrome (CP/CPPS), learning to relax the pelvic floor muscles and addressing the pain must occur before strengthening exercises are initiated.
Trapping blood in the penis, of course, will not by itself result in a rigid erection; adequate inflow of blood is equally essential. The arteries that supply the penis pass through, around, and within the muscles and connective tissues of the pelvic floor, making these tissues in a sense gate-keepers. Excess or chronic tension in the pelvic floor muscles can limit arterial inflow, thereby degrading erectile function. Skilled pelvic floor bodywork is an excellent way to stretch, release, and relax these important muscles and connective tissues — and open up the arterial pathways to enhance penile health and function.
It is important to remember that there can be many other factors that contribute to ED, among them atherosclerosis (hardening of the arteries), diabetes, hypertension, smoking, drug side effects, heavy alcohol consumption, a sedentary lifestyle, excess weight, psychological factors, and aging. The emerging field of lifestyle medicine, especially what we eat and how we move, is a powerful way to address many of these factors.Back to top
Painful Ejaculation
"I found your very informative and helpful website, and I especially appreciated your tactfulness in dealing with so sensitive a topic." - F. K.
Pain with or after ejaculation is a significant component of sexual dysfunction in men with CP/CPPS but can occur regardless of diagnosis. "Approximately half of patients with CP/CPPS have reported ejaculatory pain. ... Because patients perceive this discomfort as their response to something inflammatory or caustic in their semen, it is sometimes difficult to convince them of other possibilities such as abnormal muscular spasticity or exaggerated pelvic floor tension during orgasm" writes Potts.[11] Itza et al. agree with this perspective, reporting specific trigger points in the levator ani muscle group of the pelvic floor as being responsible for "pain during and after ejaculation." This muscle group can also refer pain to the tip of the penis and the urethra as well as to several other sites.[12] In addition, the bulbospongiosus, ischiocavernosus, and perineal muscles can contribute to ejaculatory pain.
Ejaculation triggers full, rhythmic pelvic floor contractions at 100% strength and these powerful contractions can over-challenge muscles that may already be chronically tense or otherwise compromised in some way — resulting in ejaculatory pain or discomfort. Learning to relax the muscles of the pelvic floor is thus a key goal. In addition to addressing tension, discomfort, and pain via pelvic floor massage and bodywork, I teach my clients pelvic floor relaxation tools and strategies to limit or prevent future occurrences of painful ejaculation.Back to top
Premature Ejaculation (PE)
"Ejaculatory dysfunction is one of the most common male sexual disorders" according to Rowland et al., and "various epidemiological [population] studies have shown that about 20-30% of men have complaints of premature ejaculation."[13] As in ED, weak pelvic floor muscles may play a role: "It is hypothesized that weak pelvic floor musculature affords little control to delay ejaculation and that the voluntary use of the pelvic floor muscles could delay ejaculation."[7] "Voluntary use," in this case, means learning to control when and to what degree the pelvic floor muscles contract and relax. Piediferro et al. have found manual therapy useful for premature ejaculation, stating that "...physiotherapy of the pelvic floor muscles proves successful in cases [of premature ejaculation] associated with pelvic floor dysfunction."[14]
La Pera and Nicastro evaluated treatment for premature ejaculation using a protocol to strengthen the pelvic floor muscles and increase conscious control. They found that after 15 - 20 sessions of pelvic floor
 rehabilitation, 61% of the men "were cured and able to control their ejaculatory reflex." They emphasized that "this therapy is easy to perform, has no side effects, and can be included among the therapeutic options for patients with premature ejaculation."[15]
rehabilitation, 61% of the men "were cured and able to control their ejaculatory reflex." They emphasized that "this therapy is easy to perform, has no side effects, and can be included among the therapeutic options for patients with premature ejaculation."[15]
Frank Sommer, in his book VigorRobic, writes that "men suffering from early ejaculations can delay these with the help of targeted training of the pelvic diaphragm [pelvic floor muscles]. Men who are not satisfied with the duration of their erection can also learn to control the ejaculation reflex by targeted training." Dr. Sommer's book includes exercise protocols with clear graphics, but note that the translation from the original German has a few quirks.[16]
The first step in gaining control of an area is awareness, and pelvic floor massage and bodywork is an excellent way to accomplish this. Awareness includes learning where these muscles are, what they do, and how to consciously contract them in isolation. A strength building exercise program can then be instituted to improve tone and function - and better ejaculatory control. I will guide you through this process and give you an exercise protocol for home use.
Note that addressing your pain and learning to relax the pelvic floor are necessary prerequisites if PE is associated with CP/CPPS.Back to top
Pain in the Penis
The muscles of the pelvic floor can create or refer discomfort or pain that can be felt anywhere in the penis - the base, shaft, tip, or in the urethra. This can occur independent of any diagnosis or can be part of the symptoms associated with CP/CPPS.
"I wanted to thank you for a great job. All of my [ genital ] pain is gone, as well as my groin pain." - M. S.
Travell and Simons report that "...the anterior [front] half of the pelvic floor muscles, the ischiocavernosus and the bulbospongiosus, are likely to refer pain to the genital structures... and base of the penis beneath the scrotum."[21] Anderson[28], Wise and Anderson[22], and Itza et al.[12] all write that the front portion of the levator ani muscle group as well as the bulbospongiosus and ischiocavernosus muscles can refer discomfort or pain to the shaft and/or tip of the penis.
These muscles, plus the rectus abdominis muscle in the abdomen[12] can also cause irritation or pain in the urethra. As is the case with painful ejaculation, it can be hard to grasp that there may be nothing wrong with the urethra itself when your mind is telling you it feels painful. There is of course something wrong, but the source lies elsewhere. When no evidence of an infection can be found, muscular referral should be examined as a possible cause.
In most cases of discomfort or pain in the penis caused by muscles, excess tension and the development of trigger points are the main mechanisms through which these problems occur. Massage and bodywork can be an important part of resolving these issues.
Chronic Scrotal / Testicular Pain
Various terms are used to describe this little understood condition, including chronic scrotal pain, scrotal pain syndrome, chronic testicular pain, and testicular pain syndrome. It is defined by Keoghane and Sullivan as "persistent or recurrent episodic scrotal pain associated with symptoms suggestive of urinary tract infection or sexual dysfunction" without any evidence of disease.[17] The authors describe symptoms as "a dull, throbbing, unilateral pain in the scrotum that may worsen throughout the day. The pain might radiate to the perineum and inner thigh and can be exacerbated by cycling and horse riding. ... Pain with ejaculation is sometimes described, and the symptom complex can lead to reduced libido and subsequent sexual activity."
Post vasectomy pain syndrome (PVPS) symptoms are characterized similarly, and can include "unilateral or bilateral testicular pain, which may be perceived as a constant dull ache or severe, debilitating pain, which may be exacerbated or precipitated by sexual arousal, intercourse and/or ejaculation."[29]
Mirroring the standard medical approach to CP/CPPS, antibiotics are often administered despite no infection being found. "Abundant use of antibiotics is a common therapeutic approach, assuming an infectious etiology [cause], although evidence is lacking" write Planken and colleagues.[18] Keoghane and Sullivan concur, stating that "evidence-based treatments are lacking," adding that "many patients have no identifiable cause to explain their
 discomfort."[17] Schmidt et al., in a 2008 study, concluded that there was "no evidence for the widely held belief in Chronic Scrotal Pain Syndrome representing a chronic bacterial infection. ... We conclude that the widespread use of antibiotic agents in the treatment of CSPS seems not to be justified."[19]. Even when radical interventions are done, pain is often not resolved, suggesting a source of the pain other than the testicles. Kumar et al. write that "80% of patients may continue to have orchialgia [testicle pain] despite orchiectomy [complete removal of the testicle]."[20]
discomfort."[17] Schmidt et al., in a 2008 study, concluded that there was "no evidence for the widely held belief in Chronic Scrotal Pain Syndrome representing a chronic bacterial infection. ... We conclude that the widespread use of antibiotic agents in the treatment of CSPS seems not to be justified."[19]. Even when radical interventions are done, pain is often not resolved, suggesting a source of the pain other than the testicles. Kumar et al. write that "80% of patients may continue to have orchialgia [testicle pain] despite orchiectomy [complete removal of the testicle]."[20]
Referred pain and an overactive, tight pelvic floor may be significant factors in the generation of scrotal pain. Keoghane and Sullivan write that "dysfunction of the pelvic floor muscles can lead to overactivity. This means that the muscles contract when they should relax, resulting in pain that can be referred to the scrotum."[17] Similarly, Planken et al. note "a possible relationship between chronic testicular pain and pelvic floor overactivity." They also suggest that "chronic testicular pain should be considered part of the CPPS and be treated as such."[18] Potts writes of finding "active trigger points in surrounding muscles of the lower abdomen and pelvic floor in men with chronic scrotal or testicular pain," including those with post vasectomy pain, and believes that these can be "generous contributors to ongoing pain syndromes."[29]
Beyond the role of the pelvic floor, there are muscles outside of the pelvis which can refer pain to the scrotum. These include the internal and external obliques in the abdomen, the quadratus lumborum in the low back, and sometimes the gluteus medius and minimus which span the hip joint.[21],[22]
Given the high tone and overactivity of the pelvic floor often reported in cases of chronic scrotal pain, as well as the documented ability of certain muscles to refer pain to the scrotum, massage and bodywork can be an effective approach to this condition. Awareness is always the first step, and I will help you become aware of your tension and work with you to gently stretch and relax these muscles. This will include the pelvic floor itself and those muscles outside of it that can refer pain to the testicles and scrotum.Back to top
Anodyspareunia / Male Dyspareunia: Painful or Difficult Receptive Anal Sex (Bottoming)
The term dyspareunia is defined as the occurence of pain during sexual intercourse, and it is almost always associated with women. However, a male version has been discussed in several papers and warrants further investigation. Damon and Rosser report that "based on the limited studies to date, it appears that painful receptive anal sex is a problem for a significant proportion of men who have sex with men."[23] "Male dyspareunia is a major life issue for afflicted patients and their partners" write Oommen and Hellstrom, MDs associated with Tulane University.[24] They note that underreporting symptoms is common, but "an increase in open discussion regarding sexuality among men in recent years has resulted in a larger number of men discussing dyspareunia with their primary care clinician." Others prefer the term anodyspareunia, and describe it thus: "The term anodyspareunia has been proposed to denote a novel sexual dysfunction comprising the perception of pain during receptive anal sex."[25] Painful or difficult receptive anal sex not only affects gay men; research clearly suggests that a significant and growing percentage of straight men and their partners practice or experiment with anal penetration.
An important cause of male dyspareunia is muscular tension in the pelvic floor and anal sphincters, often coupled with a lack of awareness and control — thus making it difficult or impossible to consciously relax these muscles at will. In his groundbreaking book Anal Pleasure and Health, Jack Morin writes that "in reality, for a person who desires anal pleasure, especially intercourse, the inability to relax the anal muscles is as much a problem as a man's concerns about his erections or ejaculation."[26] These anal muscles are continuous with other muscles of the pelvic floor, and contractions of them are, for most of us, inseparable from pelvic floor contractions. The same reciprocal relationship applies to relaxation, meaning that learning to relax the pelvic floor muscles will correspondingly relax the anus. Keep in mind, however, that there are other factors that can be responsible for male dyspareunia, including psychological factors, size of the penetrating object (penis, fingers, or sex toys), and lack of lubricant.
Massage and bodywork specifically directed to the anal sphincters as well as to the surrounding pelvic floor muscles is an excellent way to enhance awareness, reduce tension, and increase voluntary control of these muscles — thus making receptive anal intercourse, often called bottoming, a much more comfortable and emjoyable experience.Back to top
Pelvic Pain as Sexual Pain
Even when there are no issues with performing the physical act of engaging in sex, when pelvic pain is present, there will be diminished appreciation and pleasure from the experience. When the pain is significant, there is often no desire for sex and/or an inability to perform. As Julia Heiman suggests, "Pelvic pain is sexual pain."[27]
______________________________________________________
Research literature is increasingly confirming the important role of the pelvic floor muscles in sexual health and dysfunction. Massage and bodywork as well as pelvic floor exercises can play a significant role in managing or resolving dysfunction as noted in the above discussions, with a subsequent improvement in overall sexual function.
It is important to bear in mind that pelvic floor exercises require motivation, consistency, and a commitment of time. For some men, greater strength will help you manage your symptoms better but may not fully resolve them. They are, however, easy to do, have no negative side effects, and can have beneficial effects in other areas such as core support and urinary integrity.
→ For those men who do not live in Northern California and are unable to travel here, I offer video consultations via Zoom. See my Consultation Services page for more information.
→ My related website coremassage4men.com has additional information on sexual function, dysfunction, and genital pain which you can read by clicking on The Body's Core tab in the main menu once there.
References
Books are in bold regular text and journal articles are in bold italic text
[1] Carriere and Feldt. The Pelvic Floor. Georg Thieme Verlag 2006, page 400.
[2] Rosenbaum and Owens. The Role of Pelvic Floor Physical Therapy in the Treatment of Pelvic and Genital Pain-Related Sexual Dysfunction. Journal of Sexual Medicine 2008; 5: 513-523.
[3] Stein, Amy. Heal Pelvic Pain. McGraw-Hill, 2009
[4] Siroky and Azadzoi, in Bourcier et al. Pelvic Floor Disorders. Elsevier Saunders 2004.
[5] Sommer et al. A Conservative Treatment Option of Curing Venous Leakage in Impotent Men. European Urology Supplements 1 (2002).
[6] Colpi GM. Perineal Floor Efficiency in Sexually Potent and Impotent Men. International Journal of Impotence Research 1999; 11: 153-157.
[7] Bo et al., eds. Evidence-Based Physical Therapy for the Pelvic Floor. Elsevier 2007.
[8] Ballard DJ. Treatment of Erectile Dysfunction: Can Pelvic Muscle Exercises Improve Sexual Function? Journal of Wound, Ostomy, and Continence Nursing 1997; 24(5): 255-264.
[9] Dorey G et al. Pelvic Floor Exercises for Erectile Dysfunction. BJU International 2005; 96: 595-597.
[10] Van Kampen et al. Treatment of Erectile Dysfunction by Perineal Exercise, Electroyographic Biofeedback, and Electrical Stimulation. Physical Therapy 2003; 83(6): 536-543.
[11] Potts J, in Chronic Prostatitis / Chronic Pelvic Pain Syndrome. Shoskes D, ed. Humana Press, 2008.
[12] Itza et al. Myofascial Pain Syndrome in the Pelvic Floor: A Common Urological Condition. Actas Urologicas Espanolas 2010; 34(4): 318-326.
[13] Rowland et al. Disorders of Orgasm and Ejaculation in Men. Journal of Sexual Medicine 2010; 7: 1668-1686.
[14] Piediferro G et al. Premature Ejaculation. 3. Therapy. Archivo Italiano di Urologia 2004; 76(4): 192-198 (abstract).
[15] La Pera G and Nicastro A. A New Treatment for Premature Ejaculation: The Rehabilitation of the Pelvic Floor. Journal of Sex and Marital Therapy 1996; 22 (1): 22-26.
[16] Sommer F. VigorRobic: Increased Potency Through Specific Fitness Training. Meyer & Meyer Sport, 2002.
[17] Keoghane SR and Sullivan ME. Investigating and Managing Chronic Scrotal Pain. BMJ 2010; 341: 1263-1266.
[18] Planken et al. Chronic Testicular Pain as a Symptom of Pelvic Floor Dysfunction. The Journal of Urology 2010; 183: 177-181.
[19] Schmidt C et al. Chronic Scrotal Pain Syndrome (CSPS): The Widespread Use of Antibiotics is Not Justified. European Urology Supplements 2008 (abstract); 7(3): 159.
[20] Kumar et al. Clinical Management of Chronic Testicular Pain. Urologia Internationalis 2010; 84: 125-131.
[21] Travell JG and Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual, Vols. 1 and 2. Williams & Wilkins, 1983 and 1992.
[22] Wise D and Anderson R. A Headache in the Pelvis: A New Understanding and Treatment for Chronic Pelvic Pain Syndromes, 6th ed. National Center for Pelvic Pain Research, 2010.
[23] Damon W and Rosser BRS. Anodyspareunia in Men Who Have Sex with Men: Prevalence, Predictors, Consequences and the Development of DSM Diagnostic Criteria. Journal of Sex and Marital Therapy 2005; 31: 129-141.
[24] Oommen M and Hellstrom JG. Male Dyspareunia. 2011. available at: uptodate.com/contents/male-dyspareunia
[25] Hollows C. Anodyspareunia: a novel sexual dysfunction? An exploration into anal sexuality. Sexual and Relationship Therapy 2007; 22(4): 429-442.
[26] Morin J. Anal Pleasure and Health, 4th revised ed. Down There Press, 2010.
[27] Heiman, J. in Nickel et al. Changing Paradigms for Chronic Pelvic Pain. Reviews in Urology 2006; 8(1): 28-35.
[28] Anderson, RU in Chaitow and Lovegrove, eds. Chronic Pelvic Pain and Dysfunction: Practical Physical Medicine. Elsevier, 2012.
[29] Potts, ed. Genitourinary Pain and Inflammation: Diagnosis and Management. Humana Press, 2008.
