Chronic Prostatitis / Chronic Pelvic Pain Syndrome
Summary
Millions of men suffer from pelvic pain and related dysfunction annually. While discomfort and pain are defining characteristics, men can also experience associated sexual and urinary problems. For many years the prostate was (and often still is) wrongly assumed to be the source of the pain and dysfunction - a view that has repeatedly been disproved by medical research. The vast majority of cases are not caused by the prostate gland, and are therefore more accurately called Chronic Pelvic Pain Syndrome (CPPS) rather than Chronic Prostatitis (CP). Drugs and surgery have largely failed to alleviate symptoms or address the cause.
Current research has shown that tension and dysfunction in the muscles of the pelvic floor play a significant and often primary role in the development of this condition and its subsequent symptoms, including pain. However, "Most physicians neither appreciate nor understand the havoc that chronic tension plays in the pelvic floor." [39]. Research has also shown that massage and bodywork can be a very effective treatment.
"I used to experience extreme bouts of prostate and pelvic pain but ever since I've been coming to see you [over the last three years] I've only experienced that once." - M. D.
Read on for a detailed discussion of CP/CPPS and the value of pelvic floor massage and bodywork. Though the section titles in the next paragraph are active links, I suggest that you scroll down and read through the sections in sequence rather than skipping around. Each section builds upon the previous one and the information as a whole is written as a narrative.
Section titles are: What is CP/CPPS? ♦ The Conventional Model of Treatment - a Dismal Track Record ♦ To What Degree is the Prostate Involved with CP/CPPS? ♦ The Role of the Pelvic Floor Muscles and the Rationale for Massage and Bodywork ♦ Stress, Emotions, Chronic Tightness, and CP/CPPS ♦ and finally, Manual Therapy Approaches for the Pelvic Floor. On the right side at the end of each section there are "back to top" links to return here to the main menu.
Below the main sections you will find several "Did You Know?" boxes with additional information regarding CP/CPPS. As you read through the text, hover your cursor over citation numbers to view the source in a pop-up text box or scroll to the bottom of the page for the full list.
What is Chronic Prostatitis / Chronic Pelvic Pain Syndrome?
CP/CPPS is a condition characterized by discomfort and pain in the pelvic area, with or without associated urinary and sexual symptoms. It is surprisingly common, affecting 5 to 10 percent of the male population and accounting for nearly two million office visits per year. The term Chronic Pelvic Pain Syndrome came into use in the 1990s when the National Institutes of Health (NIH), in an attempt to more clearly define and standardize terminology, classified Prostatitis into four categories:
- Category I: Acute Bacterial Prostatitis
- Category II: Chronic Bacterial Prostatitis
- Category III: Chronic Prostatitis / Chronic Pelvic Pain Syndrome
- Category IV: Asymptomatic Prostatitis
Categories I and II are the result of infections and are treated in the standard way with antibiotics. Category IV is defined as prostate inflammation with no symptoms, and is only found incidental to other investigations.

By far the vast majority of all men diagnosed with Prostatitis are classified as having Category III Chronic Prostatitis / Chronic Pelvic Pain Syndrome. Nguyen and Shoskes note that "Almost one-third of all men during their lifetime will experience symptoms consistent with prostatitis" but that "fewer than 10% of cases of prostatitis are caused by bacteria. Category III prostatitis (CP), or chronic pelvic pain syndrome (CPPS) as it is now known, is the most common manifestation of the disease (accounting for 90% of cases) but remains the least understood." [1].
It is important to note that CP/CPPS, by definition, is not a bacterial infection, though it is often treated as such. There are no gold-standard diagnostic tests, and CP/CPPS remains a diagnosis of exclusion, meaning other possible causes of the pain and dysfunction are ruled out first. It is a syndrome (a collection of signs and symptoms that occur together), not a disease.
Discomfort and pain are the primary symptoms of CP/CPPS, which can affect any or all of the following areas: the pelvic floor, perineum, rectum, coccyx (tail bone), prostate, penis, testicles/scrotum, groin, thighs, lower abdomen, and low back. Sometimes it is difficult to describe exactly where the pain or discomfort is, especially if it feels deep inside the pelvis. Symptoms can be intermittent or constant, and wax and wane over time.
"I would like you to know that I have noticed great improvements in my physical condition from our sessions, and I am grateful for your help. You have played a crucial role in helping me recover from my condition, and I am grateful for that. ... It is clear that you are very skilled at what you do."
- A. G.
Sexual dysfunction can include painful ejaculation, premature ejaculation, erectile dysfunction, and decreased libido.
Urinary issues associated with CP/CPPS may involve discomfort or pain when urinating (dysuria), frequent voiding (urinary frequency), the need to go immediately when the urge first arises (urinary urgency), or a weak stream.
For a full discussion of the role of the pelvic floor in sexual and urinary pain and dysfunction, see my pages on Sexual Dysfunction and Genital Pain and Urinary Dysfunction.
Among the risk factors for CP/CPPS are periods of excessive stress and high anxiety, sitting in a slumped posture for prolonged periods of time, a sedentary lifestyle, extended bicycle riding, pelvic trauma, poor posture, weight lifting, anxiety related to sexual encounters, previous pelvic surgery or infection, and psychologic factors.Back to top
The Conventional Medical Model of Treatment - A Dismal Track Record
For decades the medical community - primary care physicians (PCPs), urologists, and researchers - has struggled to understand the cause of this syndrome and develop effective treatments. While progress has been made, these efforts have largely failed. "Unfortunately, physicians often misdiagnose this problem or recommend inappropriate and sometimes dangerous treatments that offer little hope of successful outcome. ... sufferers have typically endured prolonged periods with uncertain or incorrect diagnoses, multiple tests and many failed therapeutic regimens." write Moise and colleagues, specifically referring to CPPS [2]. In fact, tests beyond those that are initially done to rule out more serious pathology are not usually in the patient's interest. "Ongoing and repeated investigations for the 'cause' are associated with a worse prognosis." states urogenital and pelvic pain specialist Andrew Baranowski. [43].
Primary care and urology practices are oriented toward drug and surgery protocols, yet research indicates these approaches are rarely successful. As a result, men with chronic pelvic pain may become "frustrated and feel misunderstood. Many patients describe a sense of alienation from healthcare providers, who are perceived to be unsympathetic to their pain and disappointment." [38]. Further, when medical tests find no apparent cause for their pain, some men are told that there is nothing wrong with them, implying that their pain may be all in their head. Travell et al. emphasize that "It is all too easy for the physician to blame the patient's psyche for the inabiliy of the physician to recognize the musculoskeletal sources of the patient's pain. This wrong assumption can be - and often is - devastating to the patient. We have so much to learn about pain, especially pain from muscles" [45]. It is worth noting that the two lead authors are physicians themselves.
Drugs / Pharmaceuticals
Antibiotics, alpha-blockers, and anti-inflammatories are the most commonly prescribed classes of drugs used in the standard treatment approach to CP/CPPS. There is little research, however, to support their use.
In a 2011 paper in Current Urology Reports, Suh and Lowe state that "Traditional treatments have included antibiotics, alpha-blockers, and anti-inflammatories, but those have not proven to be efficacious therapies through many clinical trials." [3]. Anderson, in 2008, asserts that "Traditional therapy to treat these conditions has failed. This includes antibiotics, antiandrogens, anti-inflammatories, alpha-blockers, thermal or surgical therapies, and virtually all phytoceutical [plant-based] approaches." [4]. Westesson and Shoskes agree, saying "The community standard for care for this condition is abysmal..." [5]. Many studies show a response rate no better than a placebo. "Reports of successful therapy with antibiotics, alpha-blockers, anti-inflammatories, herbal preparations, or other pharmaceuticals are mainly anecdotal, and these agents have been very unimpressive when measured against a placebo in a well-designed clinical trial." state Nickel et al. [6]. Indeed, Wise and Anderson write that "Cipro, Flomax, Lyrica, and Uroxatrol [are] shown to be no better than a placebo for CPPS." [9]. In sum, all randomized, placebo-controlled trials of antibiotics in CPPS have shown no benefit. Yet...
Urologist Russell Egerdie paints a bleak picture of the current standard approach to the treatment of CP/CPPS. He writes "Antibiotics for chronic prostatitis / chronic pelvic pain syndrome? We all use them, patients expect us to prescribe them; however, is the generalized and rampant prescribing of antibiotics justified in this unfortunate patient group? The ... answer is no; at this point in time, antibiotic therapy in CP/CPPS has not withstood the test of scientific scrutiny." Despite this acknowledgement, he later adds this stark admission: "Will urologists stop prescribing antibiotics for patients with CP/CPPS? Of course not. We have little else to offer..." [7]. Note that Egerdie's intended audience is his fellow urologists and physicians, not the general public.
Potts, a leading urologist with extensive experience in treating CP/CPPS as well as an author of many research papers and books, states unequivocally that "Empirical antibiotics should be avoided. Period." [44]. Empirical antibiotic treatment in this case refers to the very prevalent trial and error antibiotic regimens that so often are the initial treatment plan, despite there being no evidence of an infection.
Surgery
"There is no definitive surgical treatment." state Bergman and Zeitlin [8]. They continue: "It has not previously and is not presently thought of as a surgical disease." Surgeries do occur, however, despite very poor success rates. Wise and Anderson observe that "we have never seen surgery be helpful for this condition as it usually complicates the condition and sometimes makes it worse." [9]. Murphy and colleagues, in a review of management strategies for chronic prostatitis, conclude that "Prostatectomies, surgical removal of the prostate, have largely been abandoned, as many men will have recurrent symptoms postoperatively." [10]. Recurrent "prostate" symptoms after the prostate has been removed should tell us something, which leads me to the next section:Back to top
To What Degree is the Prostate involved in CP/CPPS?
This is confusing to many people because the term Chronic Prostatitis is used synonymously with the more accurate Chronic Pelvic Pain Syndrome. "The labeling of chronic pelvic pain in men as "prostatitis" may well mislead both patients and physicians into thinking that the syndrome has a more limited focus and etiology [cause] than it actually may have." write Berger and colleagues. [11]. Turner et al., in the journal Archives of Internal Medicine, state that "Although labels of prostatitis and prostatodynia [prostate pain] are commonly applied to these symptoms, associated prostate disease is unproven." [12].
Further confusing the matter are those physicians who tell their patients that they have chronic prostatitis while using the more accurate term chronic pelvic pain syndrome when discussing these same cases with their colleagues. The reasoning seems to be that a diagnosis of CP suggests to the patient that the physician knows what is causing the problem (supposedly the prostate) and "blame" can be assigned, while the term CPPS suggests only pelvic pain of unknown origin. As you will see, this "unknown origin" most often turns out to be the pelvic floor muscles.
Physical examination of the prostate finds no abnormalities in most cases. Nguyen and Shoskes maintain that "The most critical component of the examination is the digital rectal examination (DRE). ... The majority of patients with CP/CPPS will have a completely normal prostate exam on DRE." [13]. Hedelin and Fall concede that the DRE is important, but they contend that it adds little guidance to diagnosis or treatment. They characterize the consistency of the gland as "variable" and conclude that "The absence or presence of tenderness should, however, not be allowed to play a pivotal role in the diagnostic procedure. That the gland is not always tender in men with CPPS/PPS is indirect evidence of the fact that an inflammation within the gland is not the cause of the condition..." [34]. "PPS", by the way, stands for Pelvic Pain Syndrome, a European designation.
"I just wanted to say how fantastic your website is! I've been directing men to your website as I think the information you give is outstanding. My patients are finding it so helpful." - H. K.
Anderson, in a 2008 paper, states unequivocally: "Urologists should eliminate the prostate organ approach to these disorders. Only 5% - 7% of any chronic prostatitis complaint yields positive pathogenic bacterial localization [an infection]. Further, the concept of inflammatory conditions of the prostate being related to chronic pain should be seriously questioned based on results of a recent national cohort study." [4].
Wise and Anderson, in their 2010 book A Headache in the Pelvis, are more emphatic: "...we want to be very clear that most cases of pelvic pain diagnosed as 'prostatitis' are not prostatitis: the overwhelming majority of diagnoses of prostatitis do not appear to be caused by any known problem of the prostate gland. Nevertheless, most urologists have continued to use the term prostatitis and treat complaints of pelvic pain and urinary dysfunction as if they were caused by an infection or inflammation of the prostate. ... The past decades of treating the prostate in such men has shown that in approximately 95% of men with symptoms, treating their prostate gland for infection or inflammation doesn't help them. ... Despite the clear scientific evidence to the contrary and almost every urologist's clinical experience of the ineffectiveness of antibiotics for nonbacterial prostatitis, it is amazing that giving antibiotics routinely for nonbacterial prostatitis is the common practice." [9].
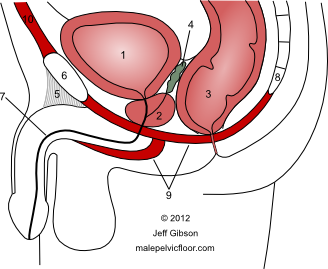
The prostate gland (2), the urethra (7), and a schematic of the pelvic floor muscles (9). See my Anatomy page for a larger size and full labeling.
Jeannette Potts, a leading urologist specializing in CPPS, sums it up well in a recent paper: "Nonbacterial prostatitis has never been proven to be a disorder of the prostate gland, much less an infectious disease. Unsurprisingly, treatments targeting an allegedly infected or abnormal prostate gland have yielded neither compelling nor consistent benefit. A more holistic and non-pharmacological [non-drug] approach to UCPPS has been long overdue." [14]. (The "U" in UCPPS stands for Urologic and expands the definition to include bladder pain).
There is no question that the prostate has a close relationship to the muscles of the pelvic floor. It rests directly on these muscles and is attached to them via connective tissues and the urethra, which courses down from the bladder through the prostate to the external urinary sphincter within the pelvic floor muscular layer. Indeed, some anatomists label specific muscle fibers in this layer as the Levator Prostatae, or "lifter of the prostate" based on what they do when they contract. As you read the next section you will see how tension and dysfunction in the pelvic floor muscles can adversely affect not only the prostate gland and genitals but also the nerves, blood vessels, and other tissues within the pelvis - and create pain throughout the region.Back to top
The Role of the Pelvic Floor Muscles and the Rationale for Massage and Bodywork
Muscles have great potential as generators of pain. In fact, common pain symptoms stem from muscular tissue more than from any other source [35]. However, this fact is often overlooked by those who view pain and dysfunction only through the prism of drugs and surgery, as Simons and Travell (both M.D.s) note in their indispensable 2-volume textbook Myofascial Pain and Dysfunction. They write: "Yet the muscles in general and trigger points in particular receive little attention as a major source of pain and dysfunction in modern medical school teaching and in medical school textbooks. This manual describes a neglected, major cause of pain and dysfunction in the largest organ [the muscles] of the body ." [36]. This is, of course, as relevant to the pelvic floor muscles as to any other muscle group.
"Jeff's bodywork session was wonderful and extremely informative. Pelvic floor issues that I have had for a long time were addressed and described in a knowledgeable and understandable way, where no one else that I have seen over these years has. I am happy to have found such a great and knowledgeable bodyworker."
- L. M
Though there were isolated voices in the medical community speaking up about the significance of the pelvic floor muscles in various pelvic pain syndromes in the last century, these voices were most often ignored. Wisniewski and Winemiller, in 2004, write "Despite the prevalence of chronic pelvic and rectal pain, the muscles of the pelvic floor are often overlooked as a source of the discomfort." [15]. The pharmaceutical industry had no interest in funding such research, and regardless, the prostate continued to be the focus of attention. Only in the last few decades has there been serious inquiry into the role of the pelvic floor muscles in causing the pain of CP/CPPS. "Pelvic floor myalgia [muscle pain] has long been suspected as the cause of symptoms attributed to prostatitis, but only recently has this suspicion been studied in a longitudinal fashion in urology." say Potts and Payne in a 2007 paper [16]. More recently, Nickel et al. state their view: "Although the pain of CP/CPPS is poorly understood, nearly all clinicians agree that almost all CP/CPPS patients have some chronic tension and tenderness of the pelvic floor musculature. It is probable that these myofascial abnormalities contribute significantly to the pain of CP/CPPS." [17]. In 2010, Westesson and Shoskes wrote "A significant extraprostatic [outside the prostate] factor in generating pain in many men with CP/CPPS is pelvic floor spasm. This muscular spasm alone can produce and mimic the pain and LUTS [lower urinary tract symptoms] of CP/CPPS." [5].
Wise and Anderson categorically state that "the source of the pain with men diagnosed with prostatitis is almost always the chronically tightened pelvic floor and not their prostate." [9]. Van Alstyne et al. agree, writing in 2010 that "According to the results of the study by Hetrick and colleagues and similar findings of Berger et al., Potts, and Weiss, CP/CPPS can be categorized as a pelvic floor muscle tension syndrome." [18].
The rationale for using massage and bodywork as a treatment for CP/CPPS is clear: the conventional model of treatment has had little success, there is no evidence the prostate is the source of the pain and dysfunction, and research clearly shows the widespread involvement of the pelvic floor muscles.Back to top
Stress, Emotions, Chronic Tightness, and CP/CPPS
What creates tension in the muscles of the pelvic floor and how does that cause the pain and dysfunction associated with CP/CPPS? Physical trauma or strain are certainly possible causes. A much more common mechanism, however, involves mental stress, emotional challenges, and past experience becoming embedded in the pelvic floor muscles in the form of tightness and rigidity. Chronic tightness and rigidity will eventually be felt as pain. For some men the pelvic floor can be a chronic tension zone, an area where their mental stress and emotional anxiety tends to get translated into physical tension. "People with chronic pelvic pain have a tendency to focus tension in the pelvic floor under stress." write Wise and Anderson [9]. Srinivasan and colleagues state that "Stress commonly exacerbates the symptoms of pelvic floor dysfunction. Pelvic floor pain is elicited similar to a tension headache." [19]. Gilbert and Glazer emphasize that "Stressful emotions can aggravate pain conditions. Denying feelings or pushing them away will not block their effects." [42]. See my Emotional and Energetic Aspects page for more on this.
When the pelvic floor muscles are tense, they create a very inhospitable environment for all the nerves, blood vessels, and organs there, as well as compromise the function of the urethra and anus. Over time, this can result in discomfort, pain, and dysfunction. Sometimes it becomes a cycle feeding on itself as tension creates pain, which causes anxiety and more tension, which creates more pain, and so forth. "Perception of pain, no matter what its cause, can lead to both reflex and voluntary muscle contraction, which may result in more pain and dysfunction." state Nickel et al. [17].
"I want to thank you. It's been nearly four weeks now that I've been almost entirely without pain. ... I appreciate all of your help." - F. K.
Another mechanism to consider is the phenomenon of referred pain. All muscles, including those in and around the pelvic floor, have the potential to develop trigger points. These are defined as "points of spot tenderness in a palpable taut band" with characteristic "referred tenderness as well as referred pain." [20]. A specific trigger point in the abdominals, for example, can refer pain to the testicle on the same side; the Adductor Magnus muscle of the inner thigh can refer pain deep within the pelvis. The pelvic floor muscles themselves can refer pain to the genitals, perineum, anus/rectum, or coccyx (tail bone). [21], [9]. The European Association of Urology's Guidelines on Chronic Pelvic Pain describes the process this way: "A muscle that is continuously contracting will ache. Nerves that pass through the pelvic floor may be compressed, and [blood] vessels to the penis and scrotum may be obstructed. Both mechanisms will lead to pelvic pain. ... Repeated or chronic muscular overload can activate trigger points in the muscle." [22].
For an account of one man's years-long journey with chronic pelvic pain and its relationship to stress, see Tim Parks' book Teach Us To Sit Still [37]. After many tests, a sadly typical progression through drug regimens, and facing surgery as a last resort, he finally finds relief (to his great surprise) through progressive relaxation, bodywork, and meditation. The author is an accomplished writer and it shows: the book is well written, engaging, and often very funny.Back to top
Manual Therapy Approaches for the Pelvic Floor
There are a variety of treatment approaches to address tension in the pelvic floor muscles. Massage and bodywork are direct ways of engaging these muscles to gently stretch and relax them, reduce or eliminate discomfort and pain, and encourage a return to proper tone and function.
Carriere and Feldt state that "Manual [hands-on] techniques are among the most basic of the treatment techniques available to physiotherapists in their approach to treatment, and they are also among the most valuable in relation to pelvic floor disorders." [41]. "Massage of the pelvic floor muscles has been established as a treatment option for these patients since reported by Thiele in 1963." write Srinivasan and colleagues [19]. Wehbe et al. found that "Physical therapy, including manual therapy and myofascial release ... offers a safe and effective form of evaluation and treatment for the patient with UCPPS." [23]. Potts adds that "The broad repertoire of techniques offered by physical therapy provides patients with a safely tailored regimen, which is both effective and empowering." [24]. And a report by Nickel et al. concludes that "Physical therapies may hold the key to ameliorization of pain and disability in patients who have developed dysfunctional myofascial pelvic pain." [6].
"I've made more progress in the four to five sessions I've had with you than I made at [a local pelvic pain clinic] in a similar amount of sessions. Our work together is really helpful."
- D. G
Note that manual techniques employed in physical therapy and physiotherapy are generally the same techniques used by well trained massage and bodywork practitioners, such as Myofascial Release, Deep Tissue Massage, Trigger Point Release, Cross-Fiber, and Neuromuscular Therapy for example. Many of these techniques address the connective tissue as well.
Even full-body massage using Swedish Massage techniques has shown promise as a treatment option for CPPS. In the only study to date in which standard massage was included (and even then, only as a comparison group, not the treatment group), the positive results for men with CPPS surprised the study authors. They concluded: "At a minimum these results suggest that therapeutic massage may merit further study as a therapeutic alternative for UCPPS." [25]. 40% of the men in the massage group were classified as responders (moderately or markedly improved) at the end of the study, which is amazing given that any work on the pelvic floor was prohibited. Needless to say, had the study design included massage that specifically addressed the muscles of the pelvic floor as well as the rest of the body it would have had the potential to be much more effective.
See my Massage and Bodywork page for more information on my approach to the pelvic floor and the modalities I use. Also visit my Maintaining a Healthy Pelvic Floor page for discussions on stress management and relaxation, physical activity, stretching, behavior modification, and other supportive measures.
NOTE: For those men who do not live in Northern California and are unable to travel here, I offer consultations via phone. See my Consultation Services page for more information.
______________________________________________________
Finally, it is important to acknowledge that many aspects of CP/CPPS remain enigmatic, and no one has all the answers. While addressing pelvic floor muscle tension may be key for some, or even most, there are men for whom this will not be the case. No one form of treatment is universally successful. Fortunately, there is little risk involved, no drug side effects, and the potential for much benefit.Back to top
Did You Know?
Daniel Shoskes, a prominent urologist in the field of Chronic Prostatitis / Chronic Pelvic Pain Syndrome, recently issued a plea to his fellow urologists to improve their diagnosis and treatment of this condition. He describes the current status this way: "Frequently, the diagnosis and management of these conditions is empiric [trial and error; not based on science], inadequate, ineffective, and contrary to the published literature of the past 10 years." He then references Martin Luther's 95 theses posted on the church door in 1517 and states that "we need a broad reformation of the medical community's management of these disorders." His "reformation" includes 23 of his own theses, in which he implores urologists to vastly improve their standard of care for CP/CPPS. Among them are:
- "Stop telling everyone that they have prostatitis as though it is one disease.", referencing the National Institutes of Health's four primary distinctions.
- "You should not tell a man with pain between his nipples and knees that he has prostatitis without doing a proper history and physcial examination.", perhaps referring to the extent that prostatitis has become a catch-all diagnosis.
- Along a similar vein, he says "Just because the patient complains of pain during a rectal exam, it does not mean that they have prostatitis."
- And he drives home an important point: "Help patients to be optimistic, because most will eventually get better. Do not tell them that this is a condition they will have until the day they die." [33].
References
Books are in bold regular text and journal articles are in bold italic text
[1] Nguyen CT and Shoskes DA, in Chronic Prostatitis / Chronic Pelvic Pain Syndrome, Humana Press, 2008. Shoskes, DA, ed.
[2] Moise G et al. Treatment of Chronic Pelvic Pain in Men and Women, Expert Review of Neurotherapeutics 2007 May; 7 (5): 507-520.
[3] Suh LK and Lowe FC. Alternative Therapies for the Treatment of Chronic Prostatitis. Current Urology Reports 2011; 12: 284-287.
[4] Anderson RU. The Role of Pelvic Floor Therapies in Chronic Pelvic Pain Syndromes. Current Prostate Reports 2008; 6: 139-144.
[5] Westesson KE and Shoskes DA. Chronic Prostatitis / Chronic Pelvic Pain Syndrome and Pelvic Floor Spasm: Can We Diagnose and Treat? Current Urology Reports 2010; 11: 261-264.
[6] Nickel JC et al. Changing Paradigms for Chronic Pelvic Pain: A Report from the Chronic Pelvic Pain / Chronic Prostatitis Scientific Workshop. Reviews in Urology 2006; 8(1): 28-35.
[7] Egerdie RB, in Chronic Prostatitis and Chronic Pelvic Pain Syndrome. Humana Press, 2008. Shoskes, DA, ed.
[8] Bergman J and Zeitlin SI. Chronic Prostatitis / Chronic Pelvic Pain Syndrome, Humana Press, 2008. Shoskes DA, ed.
[9] Wise D and Anderson RU: A Headache in the Pelvis: A New Understanding and Treatment for Chronic Pelvic Pain Syndromes, 6th edition. National Center for Pelvic Pain, 2010.
[10] Murphy et al. Chronic Prostatitis: Management Strategies. Drugs 2009; 69(1): 71-84.
[11] Berger RE, et al. Pelvic tenderness is not limited to the prostate in chronic prostatitis / chronic pelvic pain syndrome (CPPS) type IIIA and IIIB: comparison of men with and without CP/CPPS. BMC Urology 2007; 7:17.
[12] Turner JA, et al. Health Concerns of Patients With Nonbacterial Prostatitis / Pelvic Pain. Archives of Internal Medicine 2005; 165: 1054-1059.
[13] Nguyen CT and Shoskes DA, in Chronic Prostatitis / Chronic Pelvic Pain Syndrome. Humana Press, 2008. Shoskes DA, ed.
[14] Potts JM: Nonpharmological Approaches for the Treatment of Urological Chronic Pelvic Pain Syndromes in Men. Current Urology Reports 2009; 10: 289-294.
[15] Wisniewski SJ and Winemiller MH. Pelvic Floor Tension Myalgia. Practical Pain Management 2004; volume 4, issue #6.
[16] Potts J and Payne RE. Prostatitis: Infection, neuromuscular disorder, or pain syndrome? Proper patient classification is key. Cleveland Clinic Journal of Medicine 2007 volume 74; supplement 3: S63-S71.
[17] Nickel JC et al. Management of Men Diagnosed With Chronic Pelvic Pain Syndrome Who Have Failed Traditional Management. Reviews in Urology 2007; 9(2): 63-72.
[18] Van Alstyne LS et al. Physical Therapist Management of Chronic Prostatitis / Chronic Pelvic Pain Syndrome. Physical Therapy 2010; 90(12): 1795-1806.
[19] Srinivasan AK et al. Myofascial Dysfunction Associated with Chronic Pelvic Floor Pain: Management Strategies. Current Pain and Headache Reports 2007; 11: 359-364.
[20] Simons DG. Understanding effective treatments of myofascial trigger points. Journal of Bodywork and Movement Therapies. 2002; 6(2): 81-88.
[21] Travell JG and Simons DG. Myofascial Pain and Dysfuntion: The Trigger Point Manual. Vol. 2: The Lower Extremities. Williams and Wilkins 1992.
[22] Fall M (chair) et al. Guidelines on Chronic Pelvic Pain. European Association of Urology 2008.
[23] Webhe et al. Minimally Invasive Therapies for Chronic Pelvic Pain Syndrome. Current Urology Reports 2010; 11: 276-285.
[24] Potts JM, in Chronic Prostatitis / Chronic Pelvic Pain Syndrome, Humana Press, 2008. Shoskes, DA, ed.
[25] Fitzgerald et al. Randomized Multicenter Feasibility Trial of Myofascial Physical Therapy for the Treatment of Urological Chronic Pelvic Pain Syndromes. Journal of Urology 2009; 182: 570-580.
[26] Yavascaoglu et al. Role of Ejaculation in the Treatment of Chronic Non-Bacterial Prostatitis. International Journal of Urology 1999; 6: 130-134.
[27] Hedelin H and Jonsson K.Chronic Prostatitis / Chronic Pelvic Pain Syndrome: Symptoms Are Aggravated by Cold and Become Less Distressing with Age and Time. Scandinavian Journal of Urology and Nephrology 2007; 41: 516-520.
[28] Sadeghi-Nejad H and Seftel A Sexual Dysfunction and Prostatitis. Current Urology Reports 2006; 7: 479-484.
[29] Calhoun EA. Primary Care Physician Practices in the Diagnosis, Treatment and Management of Men with Chronic Prostatitis / Chronic Pelvic Pain Syndrome. Prostate Cancer and Prostatic Diseases 2009; 12: 288-295.
[30] Mishra VC et al. Role of Repeated Prostatic Massage in Chronic Prostatitis: A Systematic Review of the Literature. Journal of Urology 2008; 72(4): 731-736
[31] Pitts et al. Prevalence and Correlates of Three Types of Pelvic Pain in a Nationally Representative Sample of Australian Men. Journal of Sexual Medicine 2008; 5: 1223-1229.
[32] Lee et al. Prostate Biopsy Culture Findings of Men with Chronic Pelvic Pain Syndrome Do Not Differ from Those of Healthy Controls. Journal of Urology 2003; 169: 584-588.
[33] Shoskes DA. Commentary on Chronic Prostatitis / Chronic Pelvic Pain Syndrome: The Status Quo Is Not Good Enough (But It Can Be). UroToday International Journal 2010 June; 3(3).
[34] Hedelin H and Fall M. Controversies in Chronic Abacterial Prostatitis / Pelvic Pain Syndrome. Scandinavian Journal of Urology and Nephrology. 2008; 42: 198-208.
[35] Jantos M. Understanding Chronic Pelvic Pain. Pelviperineology. 2007; 26: 66-69. Available at pelviperineology.org
[36] Simons et al. Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 1, second edition. Williams & Wilkins, 1999.
[37] Parks T. Teach Us To Sit Still: A Skeptic's Search for Health and Healing. Rodale, 2011.
[38] Potts JM, ed. Genitourinary Pain and Inflammation: Diagnosis and Management. Humana Press, 2008.
[39] Wise D, in Potts, JM, ed. Genitourinary Pain and Inflammation: Diagnosis and Management. Humana Press, 2008.
[40] Potts JM. Alternative Approaches to the Management of Prostatitis: Biofeedback, Progressive Relaxation and the Concept of Functional Somatic Syndromes. European Urology Supplements 2 (2003) 34-37.
[41] Carriere B and Feldt CM. The Pelvic Floor. Thieme, 2006.
[42] Gilbert C and Glazer H, in Chaitow L and Jones RL, eds. Chronic Pelvic Pain and Dysfunction: Practical Physical Medicine. Elsevier, 2012.
[43] Baranowski AP, in Chaitow L and Jones RL, eds. Chronic Pelvic Pain and Dysfunction: Practical Physical Medicine. Elsevier, 2012.
[44] Potts J. American Urological Association News, July 2013. p. 9.
[45] Travell JG et al. Myofascial Pain and Dysfunction: The Trigger Point Manual. Volume 1, second edition. Williams and Wilkins, 1999.
